‘Devils Visit Angels’ at St. Joseph’s Children’s Hospital
 St. Joseph’s Children’s Hospital (SJCH) received a special visit from the New Jersey Devils this holiday season. John Moore (#2), Jiri Tlusty (#9) and Joseph Blandisi(#64) brought smiles to the children as they signed autographs and took pictures with them and their families. Among the many young patients the players met is Tafone Parker (age 15, Paterson), who is looking forward to wearing his new New Jersey Devils t-shirt.
St. Joseph’s Children’s Hospital (SJCH) received a special visit from the New Jersey Devils this holiday season. John Moore (#2), Jiri Tlusty (#9) and Joseph Blandisi(#64) brought smiles to the children as they signed autographs and took pictures with them and their families. Among the many young patients the players met is Tafone Parker (age 15, Paterson), who is looking forward to wearing his new New Jersey Devils t-shirt.
December 14, 2015
 Staff and community members came together at St. Joseph's Wayne Hospital (SJWMC) in Wayne, NJ to celebrate a special holiday tradition – the Annual Christmas Tree Lighting. The festive occasion was filled with joyous song provided by the Passaic County Technical Institute 'Tech Tone' Choir. Attendees enjoyed the dazzling lights and beautiful decorations on the tree, including (left to right) Sr. Ann Dorrity, SC, Administrative Assistant, Pastoral Care; Sr. Jeanne Agans, SC, Member, Board of Trustees, SJWMC Foundation; Daniel Kline, Vice President, SJH, and Site Administrator, SJWMC; Sr. Patricia Mennor, SC, Vice President, Mission, SJH; Fr. Martin Rooney, Director, Mission Services, St. Joseph’s Health (SJH); Ruthanne Braddock, MA, RN, NEA-BC, Site Director, Nursing, SJWMC; and Lisa Brady, Senior Vice President and Chief Operating Officer, SJH.
Staff and community members came together at St. Joseph's Wayne Hospital (SJWMC) in Wayne, NJ to celebrate a special holiday tradition – the Annual Christmas Tree Lighting. The festive occasion was filled with joyous song provided by the Passaic County Technical Institute 'Tech Tone' Choir. Attendees enjoyed the dazzling lights and beautiful decorations on the tree, including (left to right) Sr. Ann Dorrity, SC, Administrative Assistant, Pastoral Care; Sr. Jeanne Agans, SC, Member, Board of Trustees, SJWMC Foundation; Daniel Kline, Vice President, SJH, and Site Administrator, SJWMC; Sr. Patricia Mennor, SC, Vice President, Mission, SJH; Fr. Martin Rooney, Director, Mission Services, St. Joseph’s Health (SJH); Ruthanne Braddock, MA, RN, NEA-BC, Site Director, Nursing, SJWMC; and Lisa Brady, Senior Vice President and Chief Operating Officer, SJH. 
 The St. Joseph’s Wayne Medical Center Foundation is pleased to present the 2015 St. Joseph’s Wayne Medical Center Distinguished Physician Award to Michael Steinberg, MD. With two decades of service to the hospital in clinical and leadership capacities, Dr. Steinberg is highly respected for his unwavering commitment to St. Joseph’s and the surrounding communities.
The St. Joseph’s Wayne Medical Center Foundation is pleased to present the 2015 St. Joseph’s Wayne Medical Center Distinguished Physician Award to Michael Steinberg, MD. With two decades of service to the hospital in clinical and leadership capacities, Dr. Steinberg is highly respected for his unwavering commitment to St. Joseph’s and the surrounding communities.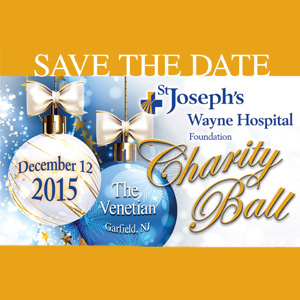 St. Joseph’s Wayne Medical Center (SJWMC) invites you to their annual Charity Ball, hosted by the hospital’s Foundation, to be held on Saturday, December 12, 2015 at The Venetian in Garfield, New Jersey.
St. Joseph’s Wayne Medical Center (SJWMC) invites you to their annual Charity Ball, hosted by the hospital’s Foundation, to be held on Saturday, December 12, 2015 at The Venetian in Garfield, New Jersey.