Meet Our Residents
Meet our current residents/ Medical school/ Preliminary year
CA 1
Cange, Tory, St. George's University School of Medicine, Zucker School of Medicine at Northwell, Peconic Bay, NY
Chokshi, Shilpan, New York Medical College, Kaiser Permanente Los Angeles Med Ctr, Los Angeles, CA
Elassa, Mohammed, Rowan University School of Osteopathic Medicine, St. Joseph's University Medical Center, Paterson, NJ
Gottlieb, Samantha, New York Institute of Technology College of Osteopathic Medicine, Lincoln Medical Center, Bronx, NY
Mullani, Naureen, Medical College of Georgia at Augusta University, Northside Hospital, Lawrenceville, GA
Parmar, Dinesh, St. George's University School of Medicine, St. Joseph's University Medical Center, Paterson, NJ
Schoenbrun, Ilana, New York Medical College, Valhalla, NY, Bronx Care Health System-NY
CA 2
Amacher, Chase, Virginia Commonwealth University School of Medicine, Virginia Commonwealth University, Richmond, VA
Bardash, Yonatan, Donald and Barbara Zucker School of Medicine at Hofstra/Northwell, Lenox Hill Hospital, New York, NY
Brown, Ashley, Rutgers Robert Wood Johnson Medical School, Griffin Hospital, Derby, CT
Chan, Rachel, New York Institute of Technology College of Osteopathic Medicine, South Nassau Communities Hospital, Oceanside, NY
Gadalla, George, Lewis Katz School of Medicine at Temple University, Abington Memorial Hospital, Abington, PA
Jezierski, Kenneth, University of Kansas School of Medicine, Wichita, KS, St. Joseph's University Medical Center, Paterson, NJ
Patel, Ronak, Marian University College of Osteopathic Medicine, Inspira Medical Center - Woodbury Program, Vineland, NJ
Shalan, Gannat, Rowan University Sch of Osteopathic Medicine, Zucker Sch of Med - Northwell/Staten Island University Hospital, Staten Island, NY
Ca 3
Albano, Jenna, Touro College of Osteopathic Medicine - New York, Mercy Catholic Medical Center, Darby, PA
Brothers, Julia, Touro College of Osteopathic Medicine - New York, Stony Brook Medicine/University Hospital, Stony Brook, NY
Badgett, Jacob, Rowan University School of Osteopathic Medicine, St. Joseph's University Medical Center, Paterson, NJ
Cabison, Kyle, St. George's University School of Medicine, Jersey Shore University Medical Center, Neptune, NJ
Fotinos, Anastasios, Rowan University School of Osteopathic Medicine, Hackensack Meridian Health - Palisades Medical Center, North Bergen, NJ
Li, Yang, Wake Forest School of Medicine, Winston-Salem, NC, Virginia Commonwealth University Health System, Richmond, VA
Riaz, Essa, St. George's University School of Medicine, New York Presbyterian - Queens, Flushing, NY
Serra, Deepthi, Rowan University School of Osteopathic Medicine, St. Joseph's University Medical Center, Paterson, NJ

 Resident/Attending Night Out
Resident/Attending Night Out New resident welcome party
New resident welcome party



 CA-1 year:
CA-1 year: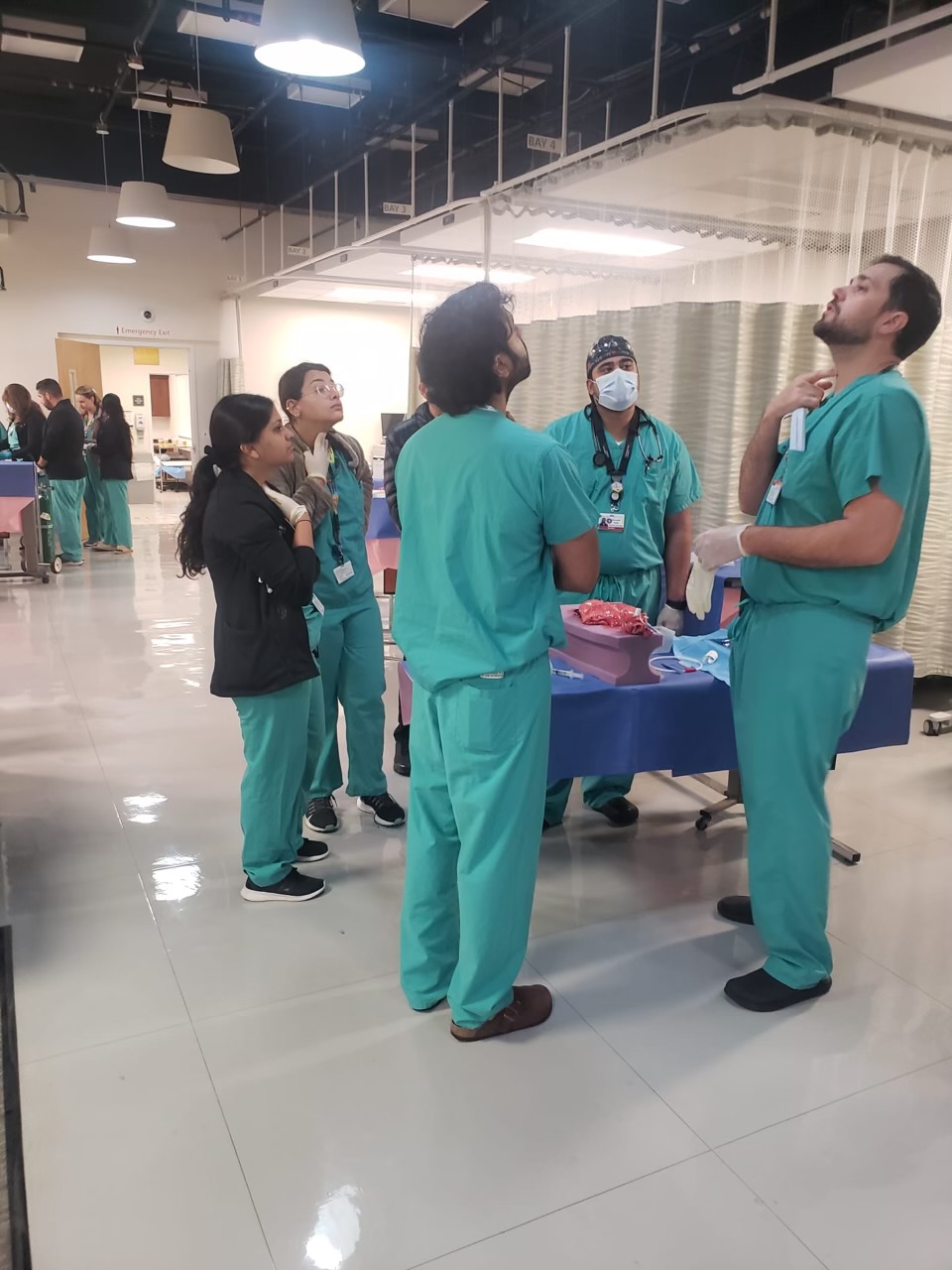 Cardiothoracic Anesthesia: (Suhaib Akhtar, Director, SJUMC< Harish Nandigam, Co-Directors, SMMC)
Cardiothoracic Anesthesia: (Suhaib Akhtar, Director, SJUMC< Harish Nandigam, Co-Directors, SMMC) Postanesthesia Care Unit :
Postanesthesia Care Unit :